Smart Insulin Patches: The Future of Diabetes Management
Diabetes is a global health challenge affecting over 500 million people worldwide. Managing this chronic condition requires constant monitoring of blood glucose levels and, in many cases, daily insulin injections. However, scientific advancements are paving the way for innovative treatment methods that aim to simplify and improve diabetes care. One of the most promising developments in this field is the smart insulin patch.
Smart insulin patches represent a revolutionary approach to insulin delivery. These devices are designed to sense changes in blood glucose levels and release insulin automatically as needed, reducing the need for multiple daily injections and minimizing the risk of hypoglycemia or hyperglycemia.

Close Up Of Diabetic Girl Sitting On Bed At Home Checking Insulin Levels On Mobile Phone App
What Is a Smart Insulin Patch?
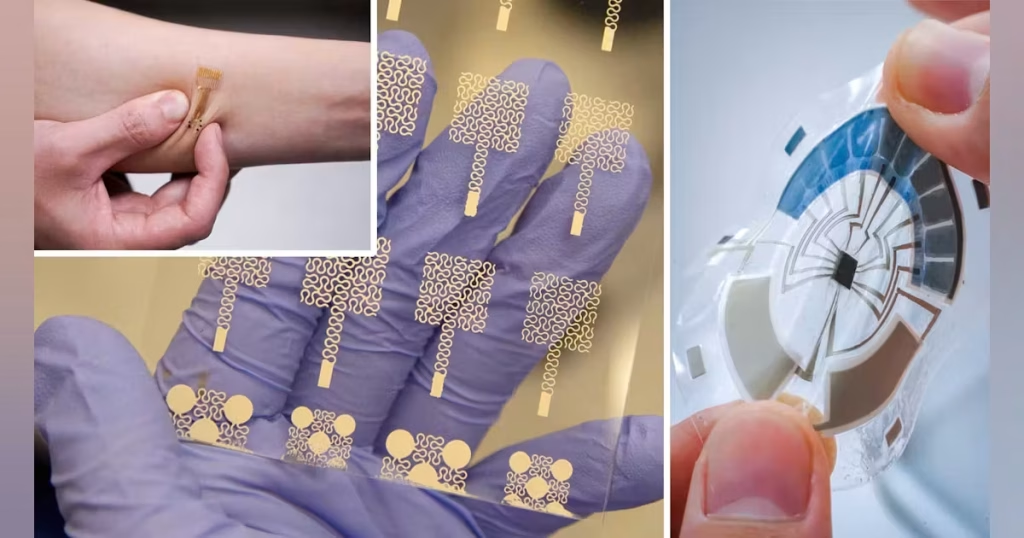
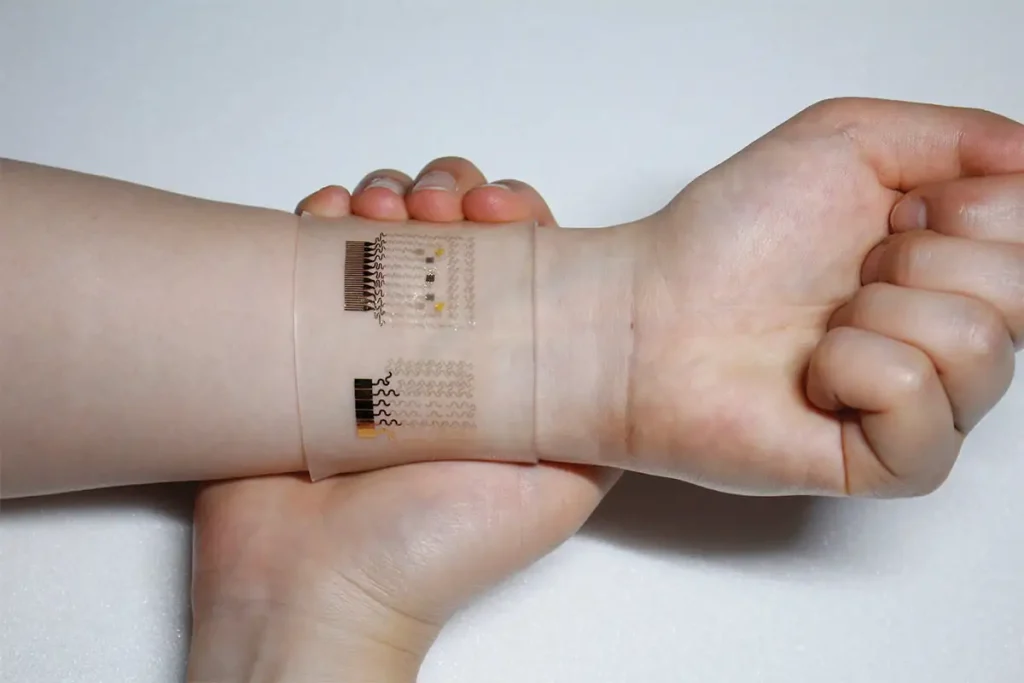
A smart insulin patch is a wearable device that adheres to the skin like a bandage. It contains tiny, painless microneedles or nanoparticle-based systems that can detect glucose levels in real-time and deliver insulin in response to those changes.
These patches are usually made from biocompatible materials and contain:
-
Microneedles: These penetrate only the uppermost layer of the skin, delivering insulin without pain.
-
Sensors: Monitor glucose levels continuously.
-
Microprocessors or smart materials: Trigger insulin release when glucose levels rise beyond a certain threshold.
-
Insulin reservoirs: Store insulin for on-demand release.
How Do Smart Insulin Patches Work?
Smart insulin patches operate on the principle of closed-loop insulin delivery — a feedback system that mimics the pancreas. Here’s how the process works:
-
Detection: The patch uses sensors to monitor interstitial glucose levels.
-
Analysis: Microprocessors interpret the glucose data.
-
Action: If glucose levels are too high, insulin is released from the reservoir via microneedles or triggered nanoparticles.
-
Regulation: The device stops releasing insulin once glucose levels normalize.
Some advanced prototypes also connect wirelessly to smartphones, enabling patients and healthcare providers to track glucose trends and device activity.

Advantages Over Traditional Methods
Smart insulin patches offer numerous benefits over conventional diabetes treatments:
1. Minimized Injections
Smart patches eliminate the need for multiple daily insulin injections, making treatment less invasive and more convenient.
2. Real-Time Glucose Monitoring
Many patches include continuous glucose monitoring (CGM), giving users up-to-date readings without finger-prick tests.
3. Precision Delivery
The patch only delivers insulin when needed, reducing the risk of incorrect dosing and avoiding both hyperglycemia and hypoglycemia.
4. Improved Compliance
With fewer manual steps required, patients are more likely to adhere to their treatment plans.
5. Reduced Pain and Discomfort
Microneedles are much smaller than traditional needles, often too small to activate pain receptors.

Scientific Innovations Behind Smart Insulin Patches
There are several types of smart insulin patches under development, each utilizing different cutting-edge technologies:
1. Microneedle-Based Patches
These use microscopic needles that dissolve or retract after insulin delivery. They can be made of materials like hyaluronic acid, which safely biodegrades in the skin.
2. Glucose-Sensitive Polymers
Some patches incorporate materials that change shape or permeability in response to high glucose levels, enabling insulin to diffuse passively when needed.
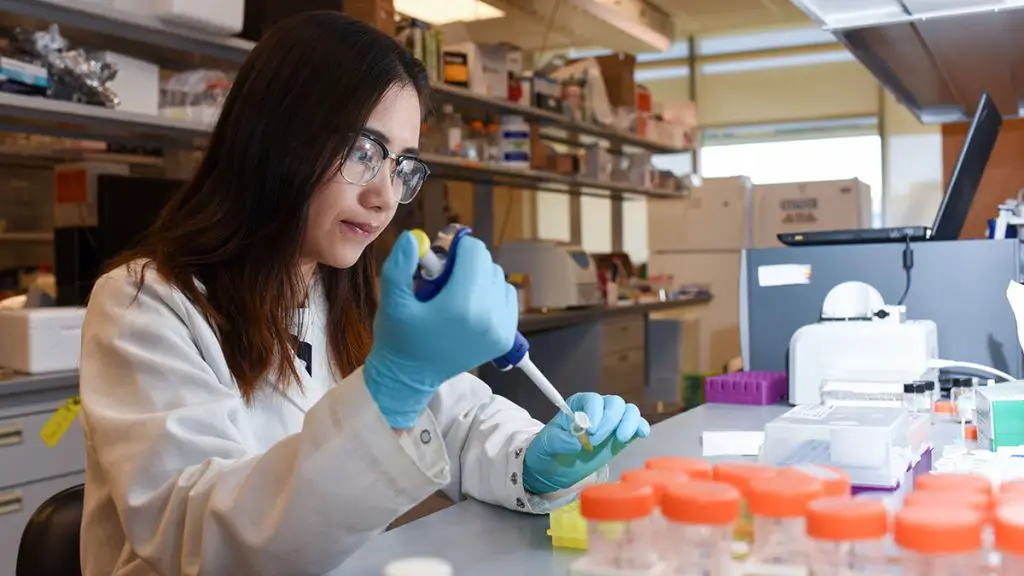
3. Enzyme-Triggered Systems
These patches use glucose oxidase, an enzyme that reacts with glucose to produce a small electric signal or trigger a chemical change that releases insulin.
4. pH-Sensitive and Thermo-Responsive Hydrogels
As blood glucose levels rise, chemical reactions in these patches alter their physical state to release insulin.
Current Research and Clinical Trials
Smart insulin patch research is being conducted worldwide, with several prototypes showing great promise.
Notable Projects:
-
University of North Carolina & NC State University (USA): Developed a patch with insulin-loaded microneedles activated by rising glucose levels. In preclinical trials, it successfully regulated blood sugar in diabetic mice for over 9 hours.
-
MIT (Massachusetts Institute of Technology): Designed a hydrogel patch responsive to both glucose and pH levels, offering dual control for precision insulin release.
-
Chinese Academy of Sciences: Created a wearable patch integrating both glucose sensors and microneedles, capable of delivering fast and long-acting insulin.
These innovations are undergoing animal testing and early-phase human clinical trials. Regulatory approval is still pending, but results so far are promising.

Challenges and Limitations
While smart insulin patches offer a glimpse of a better future for diabetes care, they are not without hurdles:
1. Biocompatibility and Safety
Ensuring the materials used in the patches are non-toxic and do not cause allergic reactions is a major concern.
2. Manufacturing and Cost
Mass-producing patches with advanced microelectronics and nanomaterials must be cost-effective to ensure accessibility.
3. Insulin Stability
Insulin must remain stable within the patch at body temperature over extended periods, which is a challenge for many designs.
4. Regulatory Approvals
Like all medical devices, smart insulin patches must go through rigorous testing to gain FDA and other global health regulatory approvals.

The Future Outlook
The future of smart insulin patches looks bright. As technology advances, we can expect:
-
Longer wear durations (currently around 1–2 days).
-
Integration with AI-powered health monitoring platforms.
-
Greater affordability and wider accessibility.
Researchers are also working on closed-loop systems, often referred to as “artificial pancreas” devices, where smart patches work in tandem with CGMs and smartphone apps to completely automate diabetes care.
Conclusion
Smart insulin patches could fundamentally change how diabetes is managed. By offering pain-free, automatic, and accurate insulin delivery, these devices have the potential to improve patient quality of life, reduce the burden of disease, and enhance overall treatment outcomes. While still in the development stage, ongoing research and clinical trials suggest that these innovative patches may soon become a standard part of diabetes management.
As we move toward a more connected and health-conscious future, smart insulin patches represent a powerful symbol of how engineering, biotechnology, and medicine can come together to solve real-world problems.








